Box 32: What You Need to Know.
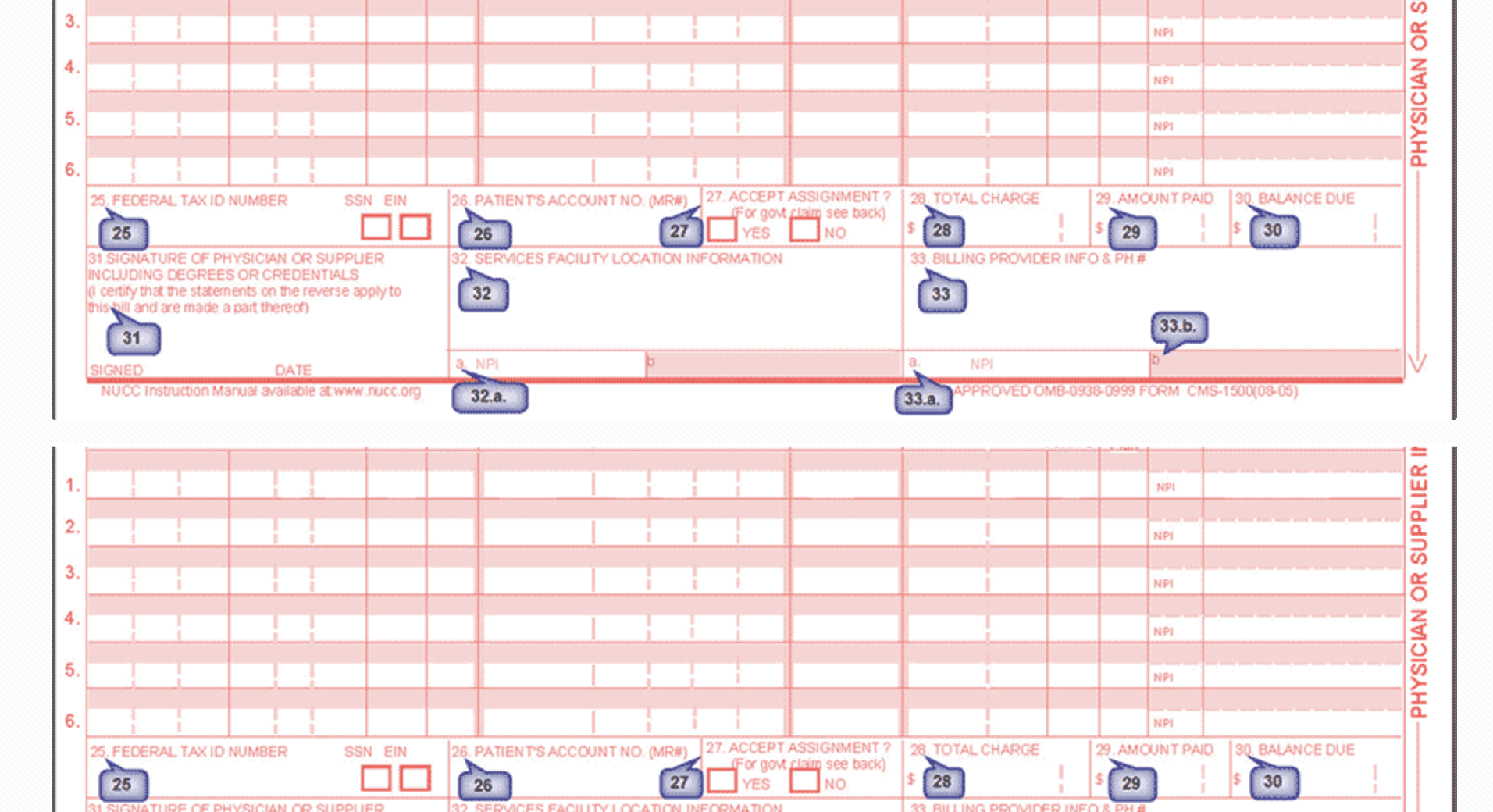
Box 32 on Medicare and Medicaid reimbursement forms is critical when billing for telehealth services, as it captures the "service facility location information" — aka where the place where the service is rendered. For telehealth claims, Box 32 reflects the originating site where the patient is located, which may be different from the provider's location listed in Box 33 (billing provider). Accurate completion of Box 32 ensures that telehealth claims align with CMS policies, which often dictate reimbursement based on the patient’s site of service. Below is an expanded explanation of Box 32 requirements, alongside an analysis of state-specific restrictions ranked from most restrictive to least restrictive.
Key Details About Box 32 for Telehealth:
Originating Site Requirements:
For Medicare, the originating site must generally be a healthcare facility located in a Health Professional Shortage Area (HPSA) or a non-Metropolitan Statistical Area (non-MSA). Some flexibilities introduced during the COVID-19 public health emergency (PHE) allow originating sites to include the patient's home in certain cases. However, incorrect use of Box 32 can result in claim rejections or audits. Medicaid policies for Box 32 vary significantly by state and often impose restrictions based on modality, provider type, or service location
Medicare Requirements:
The originating site listed in Box 32 must meet eligibility criteria, which traditionally included rural healthcare facilities or specific areas under a Health Professional Shortage Area (HPSA).
Flexibilities during the COVID-19 PHE expanded these sites to include the patient's home for certain services.
The Calendar Year 2024 Physician Fee Schedule allows some expanded telehealth flexibilities, but the rules are not uniform across states.
Medicaid Variations:
Medicaid rules vary widely across states, with some imposing stricter restrictions on telehealth services, modalities, or originating site eligibility.
Ranking of States by Telehealth Restrictions (Most to Least Restrictive):
Most Restrictive States:
Texas:
Limits telehealth services to synchronous (real-time video).
Medicaid does not consistently cover asynchronous modalities like store-and-forward or remote patient monitoring (RPM).
Alabama:
Reimburses only for specific services and modalities; restricts audio-only telehealth except in limited cases.
Originating site must be approved, limiting patient home use.
Mississippi:
Restricts telehealth to rural and underserved areas unless legislative exemptions apply.
Ohio:
Excludes asynchronous modalities and restricts coverage for certain specialties.
New York:
Medicaid reimburses telehealth broadly but excludes specific modalities like store-and-forward unless part of a pilot program.
Moderately Restrictive States:
North Carolina:
Expands telehealth reimbursement but limits audio-only care and RPM eligibility.
Georgia:
Allows more telehealth services under Medicaid but restricts some specialties and conditions eligible for RPM.
Florida:
Supports telehealth but imposes strict licensing requirements for out-of-state providers.
Least Restrictive States:
California:
Comprehensive coverage for Medicaid telehealth services, including asynchronous care and RPM.
Maryland:
Expands telehealth coverage but excludes some specialties from reimbursement.
Oregon:
Broad coverage under Medicaid, including audio-only and RPM, with fewer originating site restrictions.
Massachusetts:
Medicaid includes nearly all telehealth services, embracing audio-only, video, and asynchronous care without geographic restrictions.
Implications of Box 32 Mismanagement:
Reimbursement Delays: Failure to properly designate the originating site can lead to claim rejections.
Audit Risks: Non-compliance with state or federal telehealth requirements can trigger audits.
Access Barriers: States with stricter policies disproportionately impact rural and underserved populations who rely on telehealth.
Advocacy and Policy Recommendations:
To address the disparities and challenges:
Standardize Medicaid Policies: Advocating for federal guidelines under initiatives like the Telehealth Modernization Act would reduce inconsistencies.
Expand Reimbursement Models: Encourage states to adopt broader telehealth coverage, including all modalities.
Educate Providers: Support training on compliance requirements for Box 32 and other billing complexities.
Consistent policies and legislative support can ensure telehealth remains a viable and accessible option for all patients.
Challenges and Opportunities:
States differ in their Medicaid telehealth policies. For example, some restrict reimbursement to live video encounters (e.g., Ohio), while others (like Maryland) exclude certain specialties from coverage under asynchronous (store-and-forward) telehealth. Remote patient monitoring (RPM), another telehealth modality, is reimbursed in only 26 states and often has strict criteria regarding conditions and provider types
To reduce barriers, advocating for consistent federal standards, such as through the Telehealth Modernization Act, would streamline billing processes and improve equitable access to telehealth services. Expanding CMS's telehealth waivers through legislative actions could also address inconsistencies in Box 32 requirements across state Medicaid programs. This would ensure that providers can meet compliance standards while maintaining quality telehealth care.

